How to manage OCD symptoms
Learn more about how to challenge unhelpful thoughts and behaviours related to OCD.
If you have found this page, you or someone you care about may be struggling with obsessive-compulsive disorder (OCD) or obsessive-compulsive symptoms. These symptoms may include intrusive, unwanted thoughts, urges or images, also known as obsessions. In this factsheet, you will learn more about how to manage, and possibly even reduce, your obsessive-compulsive symptoms. You will also find out more about how to support someone who is experiencing these symptoms.
This factsheet covers the following areas:
How to break the OCD cycle
Unhelpful thoughts that keep the cycle going
Challenging unhelpful thoughts
Unhelpful behaviours that keep the cycle going
Challenging unhelpful behaviours
What are the symptoms of OCD?
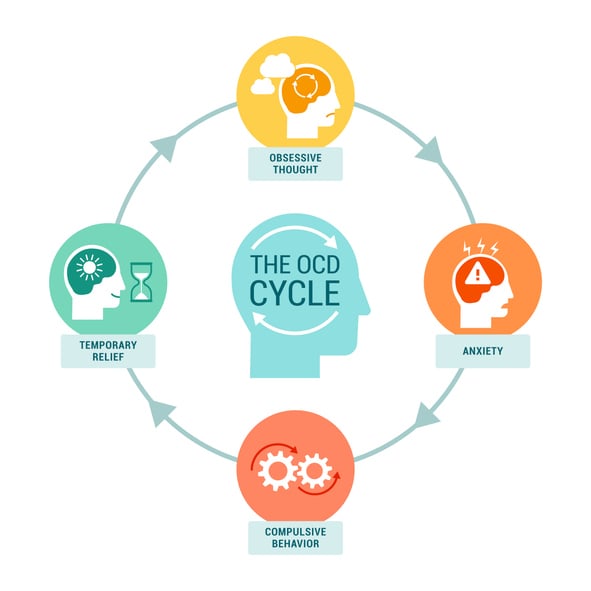
People with OCD often try to control their obsessions by performing rituals or repetitive actions. While compulsions may reduce anxiety in the moment, they are an unhelpful long-term coping strategy. This is because they can cause the cycle of OCD to repeat itself. To learn more about obsessions and compulsions, take a look at our factsheet on the common signs and symptoms of OCD.
Here’s how the OCD cycle works:
- Trigger: You come across something that triggers your OCD, like a certain situation, place, or object
- Obsession: This trigger brings about an unwanted urge, image or thought
- Unhelpful Meaning/Interpretation: You give this obsession a special meaning or interpret it in a particular way
- Increased anxiety: This special meaning or interpretation makes you feel very anxious
- Ritual or compulsion: To reduce this anxiety, you perform a ritual or a set of rituals, like checking or counting
This cycle repeats, keeping the OCD going.
How to break the OCD cycle
The special meaning a person gives to an obsession comes from how they understand or interpret it. Unhelpful interpretations of obsessions keep the OCD cycle going. For example, while driving, someone with OCD might have intrusive, unwanted thoughts such as ”I could hit that pedestrian with my car.” The meaning they attach to this thought, an unhelpful interpretation, could be: “I am a dangerous person.”
Breaking the cycle of OCD requires challenging the meaning of these unhelpful thoughts. In general, there are two main approaches to do this:
Direct Challenge:
- Question whether your thoughts are accurate and match reality
- Ask: “Am I seeing the situation as it really is, or as I fear it might be?”
Indirect Challenge:
- Reduce and gradually eliminate patterns of rituals or compulsions
- This is often done through a type of cognitive behavioural therapy (CBT) called Exposure and Response Prevention (ERP) therapy, where a person slowly exposes themselves to your triggers and learns to resist the urge to perform rituals
Unhelpful thoughts that keep the cycle going
While no two people with OCD think in the same way, there are similarities in the types of unhelpful thoughts that can lead to compulsions. Some common patterns of unhelpful thinking among people who live with OCD include:
- Exaggerated sense of responsibility: Feeling anxious about being blamed if something bad happens. For example, you might feel responsible if a person becomes ill after shaking your hand
- Overestimating threats: Feeling certain that something bad will happen in situations of potential risk. One example is believing that if you forget to lock the door your house will definitely be burgled
- Underestimating one’s ability to cope with anxiety: Feeling overwhelmed by anxiety from an obsession and doubting your ability to cope without performing familiar rituals or compulsions
- Intolerance of uncertainty: Feeling the need to constantly check, ask for reassurance, or gain more information to achieve absolute certainty and calmness about something
- Magical thinking: Believing that your thoughts can cause bad things to happen in the outside world. One example is believing that having an intrusive thought about hurting someone is as bad as actually harming them
Challenging unhelpful thoughts
Understanding your unhelpful interpretations of obsessions is the first step to challenging them. When you track your obsessions and the meanings you assigns to them, you can get to know your patterns of unhelpful thinking. This applies equally to a loved one or someone you may be supporting who experiences obsessive-compulsive symptoms. Once you or the person you are supporting has tracked their most frequent obsessions and the meaning they give to them, it can become easier to identify unhelpful patterns of thinking when they arise.
It can be difficult to identify and challenge unhelpful thoughts on your own. If you or someone you care for has been diagnosed with OCD and is experiencing obsessive-compulsive symptoms that disrupt daily life, seeking support from a clinical psychologist or CBT therapist can be really beneficial.
Unhelpful behaviours that keep the cycle going
It’s important to recognise the patterns of behaviours that make it harder to overcome obsessive-compulsive symptoms.
Below are some behaviours that can reinforce the OCD cycle. While these behaviours may seem like effective coping strategies in the short term, they tend to increase a person’s anxiety in the long term.
Rituals
Rituals, while they may temporarily relieve your anxiety, actually increase distress in the long run by:
- Preventing reality testing: Rituals can prevent you from testing whether the special meaning you assign to obsessions are real
- Undermining confidence: You may believe that you cannot survive or tolerate the anxiety your obsessions cause
- Blocking coping skills: If you always rely on rituals, they reinforce the belief that you cannot handle anxiety without them
- Distorting perception: Rituals may convince you that the level of anxiety you are feeling is proportional to the trigger when it’s not. This can make you think that extreme anxiety is a normal reaction to something minor (e.g., touching the outside of a bin)
Reassurance
When trying to resist the urge to perform a ritual, you or the person you care about might seek reassurance from others about your anxiety. For example, if you’re worried about not having checked the oven enough times, you might ask someone else at home to check it for you. Or you might look for reassurance about the meaning of an intrusive thought, such as confirmation that you are not in any danger. By doing this it can seem like you’re avoiding compulsions, but in fact, you’re not. Asking for reassurance is often considered an “indirect ritual.” It achieves the same goal as directly performing the ritual and often reinforces the special meanings you have given to intrusive thoughts. Doing this can stop you from addressing and changing these unhelpful thoughts.
Avoidance
Avoiding situations that trigger obsessions can keep the cycle of OCD symptoms going. Avoidance behaviours can:
Prevent someone proving a thought is not true
Avoiding an action stops someone from learning that an intrusive thought isn’t true. However, by doing something and there not being negative consequences, such as touching the outside of a bin and not becoming sick, a person can learn from their experience.
Reduce overall functioning
Avoiding certain activities or environments can reduce a person’s overall functioning. People may find that they are unable to perform necessary everyday tasks. They might try to give these tasks to others such as avoiding cooking to avoid the anxiety of repeatedly checking the stove.
Increase stress for others
Relying on others to help us avoid certain feared situations can add to other people’s workload and stress levels. This may cause the person experiencing the obsessive-compulsive symptoms to feel guilt or worry.
Challenging unhelpful behaviours
In general, challenging unhelpful interpretations of obsessions and breaking the OCD cycle requires a change in a person’s thinking. However, it also means a change in behaviour, especially in how much a person relies on compulsions. The most common method for doing this is Exposure and Response Prevention (ERP), a type of cognitive behavioural therapy (CBT). ERP works by interrupting the OCD cycle, and is widely accepted as being the best treatment available for OCD.
Sometimes, people choose to take steps towards addressing their obsessive-compulsive symptoms on their own. NHS Inform has published a self-help guide that includes self-directed activities and tips on practising exposure techniques.
However, exposure techniques are best performed under the care and supervision of a trained mental health professional. Professionals can create a treatment for your unique needs and challenges. When carried out alone, exposure exercises are not the same as structured ERP. Exposure exercises that are not delivered by a trained mental health professional can carry risks. Working with a suitable professional offers the highest chance of success. It helps prevent unintentionally increasing one’s levels of fear and anxiety.
Feeling overwhelmed and want to talk to someone?
- Get anonymous support 24/7 with our text message support service
- Connect with a trained volunteer who will listen to you, and help you to move forward feeling better
- Free-text SPUNOUT to 50808 to begin
- Find out more about our text message support service
If you are a customer of the 48 or An Post network or cannot get through using the ‘50808’ short code please text HELLO to 086 1800 280 (standard message rates may apply). Some smaller networks do not support short codes like ‘50808’.