The coil: What is the difference between an IUD and an IUS?
Learn more about the different types of contraceptive coil
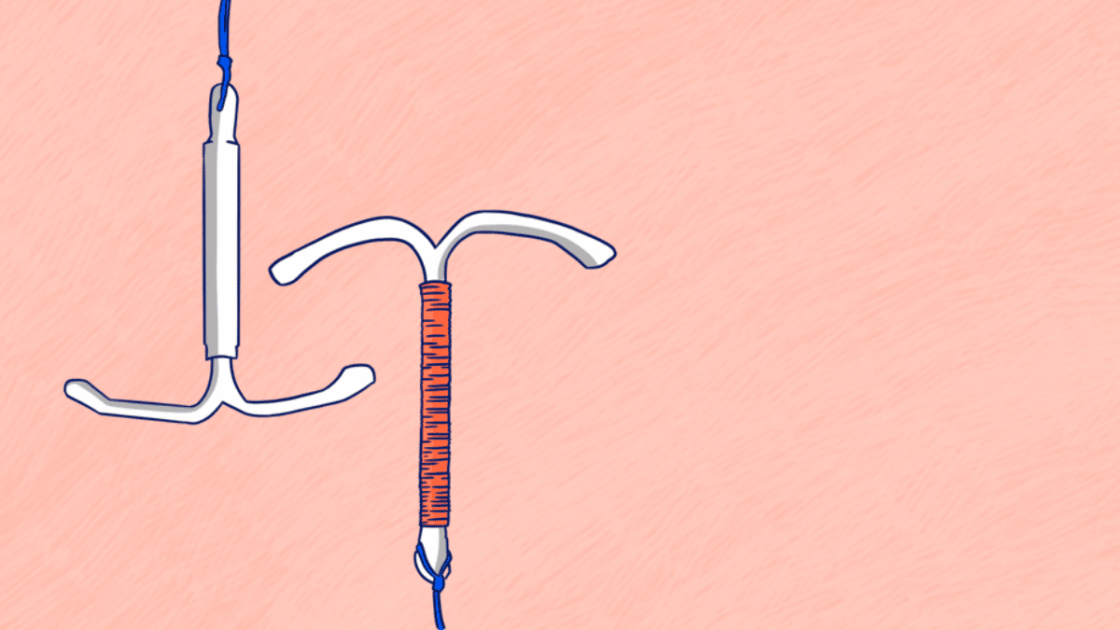
The coil, also known as an IntraUterine Device (IUD) or an IntraUterine System (IUS), is a small, T-shaped device made of either plastic or copper that is inserted into the uterus and used as a form of contraception. Depending on the device you get, it will release either copper (IUD) or a hormone called progestogen (IUS) to prevent pregnancy.
The coil is inserted by a doctor or nurse and lasts anywhere between three to ten years, depending on which type or brand you get. It can easily be removed at any time. The main difference between the IUD and the IUS is that one releases copper (IUD) and one releases hormones (IUS).
How does the coil work?
Both the IUD and the IUS work in similar ways to prevent pregnancy.
IUD
The IUD is a copper coil that prevents pregnancy by stopping sperm from reaching the egg by releasing tiny amounts of copper into the body, which is toxic to sperm and eggs. The sperm dies in a copper rich environment, and the egg can’t move properly. The copper alters the cervical mucus, meaning it changes the make-up of fluid in the womb and fallopian tubes, preventing the sperm from fertilising the egg. The copper coil can also delay the egg reaching the womb and prevent the egg from implanting in the womb.
IUS
The IUS is a hormonal coil that prevents pregnancy by releasing the hormone progestogen into the womb to thicken the cervical mucus and prevent sperm from meeting the egg. The coil can also delay the egg reaching the womb and prevent the egg from implanting in the womb. The IUS can also stop ovulation for some people, while for others ovulation will continue as usual.
The three types of IUS available in Ireland are: Mirena and Kyleena, which last for five years, and Jaydess, which lasts for three years.
How hormones work in the IUS
Unlike with the contraceptive pill or other forms of hormonal contraception, the hormones in the IUS are “local”, which means they only work within the area of your uterus. This means the hormones are less likely to have an impact on your mood or cause other physical symptoms that might occur with other hormonal contraceptives.

How effective is the coil?
Both the IUD and the IUS are 99% effective in preventing pregnancy. They begin working as soon as they have been inserted. However, neither can prevent sexually transmitted infections (STIs), so it’s also important to use a condom.
If inserted up to five days after unprotected sex, the copper coil can also be used as a form of emergency contraception, and then it can be left in as an ongoing form of contraception. This is currently only done with the copper coil (IUD). If you do want to use the coil as emergency contraception, keep in mind that it is a long term contraceptive solution, unlike the emergency contraceptive pill which is a one-off solution.
Can I use the coil?
The coil is suitable for most people, including those who have never been pregnant and those who are HIV positive.
The coil may not be suitable for you if:
- You have an untreated STI or pelvic infection
- There are any problems in your womb or cervix
- You are experiencing unexplained bleeding from your vagina in between periods or after sex
It’s best to discuss your medical history with your doctor to make sure the coil is right for you.
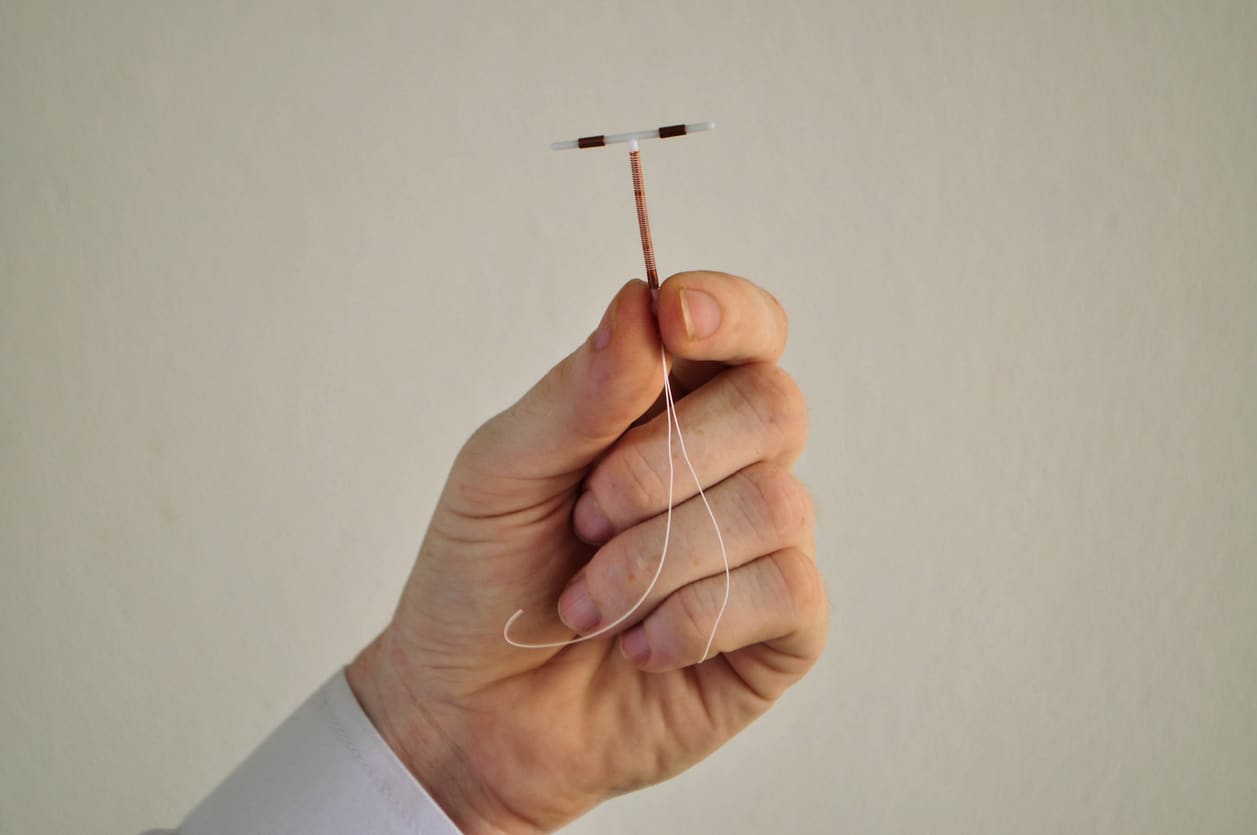
How is the coil fitted?
It is a good idea to arrange a consultation with your doctor or family planning clinic in advance of getting the IUD/IUS fitted so that you get a chance to discuss which coil would be best for you and what the best time to insert it would be.
Both the IUD and the IUS need to be fitted by a trained nurse or doctor. Before fitting, they will do a number of exams and tests, including:
- Checking the size and position of your womb
- Checking for any possible STIs and treating any infection with antibiotics
If you are checking for any infections, it’s best to arrange this before the day you plan to fit the IUD so that there is time to treat it in advance. You may still be able to have the coil inserted at the same time as having your STI screening, and get treatment later if the tests come back positive.
The procedure
In all, the procedure takes about 15-20 minutes. The vagina will be held open with a small speculum, the same way as during a smear test, and the coil is inserted through the cervix into the womb.
You will need to go to your doctor or go back to the clinic where the coil was fitted six weeks after the procedure to make sure it hasn’t moved and to make sure you aren’t having any problems
Does getting the coil hurt?
Some people do experience some minor discomfort or pain when having the coil fitted. In most cases, a person might feel a cramp when the coil is inserted, and some experience mild cramps for a number of hours afterwards.
If you are concerned about the pain, discuss this with your doctor or nurse in advance. It is recommended that you take a painkiller like ibuprofen one hour before the procedure.
After your fitting, you may experience period-like cramping pain and have some bleeding or spotting. This may last for a few days after the coil has been inserted.
If you experience any of these symptoms after having the coil fitted, you should return to your doctor, as you may have an infection:
- Feeling unwell
- Have pain in your lower abdomen
- Have a temperature
- Have smelly discharge
How is the coil removed?
The coil can be removed at any time. You will need to return to your doctor or nurse to have it removed. The procedure is very simple and much quicker and easier than having it inserted.
If you have the coil removed but you don’t want to get pregnant, it’s important that you have another form of contraception available straight away. Speak to your doctor about alternatives to the coil. Normal fertility should return immediately once the coil has been removed.
How does the coil affect your period?
The way that the coil affects your period is different for everyone, and can depend on the type of coil you had fitted.
IUD and periods
The IUD may cause heavier periods that may last slightly longer in the first few months, but not always.
IUS and periods
The IUS can cause irregular periods, light irregular spotting, or sometimes stop periods altogether. This is not harmful at all but can take some getting used to.

Benefits of the contraceptive coil
There are many benefits to choosing the contraceptive coil:
- The coil is a longer term method of contraception, lasting anywhere between three and ten years depending on the type of coil you use
- It starts working to prevent pregnancy as soon as it has been fitted
- Normal fertility returns once it has been removed
- The coil is safe to use while breastfeeding
- The coil is not affected by other medicines in the same way that other forms of contraception like the pill might be
Things to keep in mind with the coil:
- There is a small risk of pelvic infection within the first 20 days of having the coil inserted
- There is a small chance the coil could move or could be rejected and expelled from the womb soon after being fitted
- In rare cases, the coil can poke through the womb when it is inserted, which can cause pain in the lower abdomen and the coil will have to be removed
- Although the coil is 99% effective, if it happened to fail and you became pregnant, there is a risk of ectopic pregnancy, which means the egg implants itself outside of the womb and the pregnancy won’t be able to develop – this can cause a risk to your health
- You can have the coil fitted two weeks after a medical abortion, or on the day of a surgical abortion. If you would like to have the coil fitted on the day of your surgical abortion, you can get one from your doctor and bring it with you to the procedure.
If you are considering the coil, discuss this with your doctor so they can help you to make the best decision to suit your needs.
Protecting your sexual health when on contraception
If you chose to go on the coil, this will only help prevent pregnancy, but you will still need to protect yourself from STIs and HIV. There are many great options to help protect your sexual health, but none of them are 100% effective. Even if you use condoms every time you have penetrative sex, you are still at risk of getting genital warts and herpes, as these can be passed through skin-to-skin contact. Going for an STI check or taking a home STI testing kit with a partner before having sex, can be a great way of protecting yourself and those you have sex with against STIs and HIV. However, not all STI checks check for all STIs, so it is important to speak to your healthcare provider and ask them what are being tested for as part of your screening.
Discussing with your sexual partners the type of contraception or protection options available to you, and agreeing on a type that works for everyone involved can help to reduce the risk of pregnancy, STIs and HIV. Looking out for sores or symptoms on a partner’s genitals before having sex with them, can help to identify STIs that they may not be aware of. If you do see any signs that someone may have an STI, do not have sex with them until you know for certain it is safe to do so. Asking someone about their sexual health history is the responsible thing to do before having sex, and it should not be taken as an insult if someone asks you about yours.
Feeling overwhelmed and want to talk to someone?
- Get anonymous support 24/7 with our text message support service
- Connect with a trained volunteer who will listen to you, and help you to move forward feeling better
- Whatsapp us now or free-text SPUNOUT to 50808 to begin.
- Find out more about our text message support service
If you are a customer of the 48 or An Post network or cannot get through using the ‘50808’ short code please text HELLO to 086 1800 280 (standard message rates may apply). Some smaller networks do not support short codes like ‘50808’.